DENTAL HEALTH
TEETH, BONES, OSTEOPOROSIS
[From: www.dent.nihon-u.ac.jp/publ/ journal/journal46-1/P045-050.pdf }
Restorer of teeth with eroded enamel - Chemfill II Glass Iononomer Cement - Studies comparing this with other coatings, (such as Compoglass F, or Dyract AP) showed the Glass Ionomer Cement to be the superior at preventing caries. -www.dent.nihon-u.ac.jp/publ/ journal/journal46-1/P045-050.pdf
---------
[http://www.healthytomorrow.com/DentalCare.htm ]
Casein is a natural protein found in milk that has demonstrated effectiveness in preventing tooth decay. Casein remains the only natural food constituent known to improve the ratio of good bacteria-to-bad bacteria in the mouth. Casein has also shown it can prevent decay-causing bacteria from attaching to teeth. Rich in bioavailable phosphates and calcium, it also supports the remineralization of tooth surfaces. Studies have shown that casein solution is as effective as 500 ppm fluoride in aiding the prevention of cavities.
Calcium glycerophosphate is a natural constituent found in the human body. It helps prevent cavities through enzymatic cleansing. Calcium glycerophosphate complements casein in promoting the remineralization of tooth enamel.
[CALCIUM - Milk, Sources, Impediments, Etc.]
calcium carbonate supplements--even when taken with food--were still not as well absorbed as the calcium citrate.
Very high doses from calcium supplements (in the range of 2,500 mg a day) can cause kidney stones, a complication apparently due to dehydration. Be sure get plenty of fluid when taking calcium at any dosage level.
----------
Sources of calcium - broccoli, leafy vegetables such as spinach, legumes (including soybeans, peanuts, and pinto beans), almonds, brazil nuts, sesame seeds, some fish like canned salmon & sardines with the bones, firm tofu, molasses, figs, kale, bok choy and chard.
Sufficient amounts of vitamin D are made in your body when your skin is exposed to sunlight for about 10-15 minutes.
----------------
Vitamin B6 strengthens teeth...caffeine leaches calcium from your bones...higher dairy product consumption was associated with increased bone fracture risk....Exercise, so calcium has somewhere to go....It's not enough to get calcium into your bones. What is really critical is keeping it there...A lower than normal amount of testosterone can encourage osteoporosis...
-------
Bones are constantly breaking down and building up. At the age of 30-40, people's bones don't grow like they used to. So people need to do all they can to prevent this. Don't eat excess protein, cut salt intake, cut out caffeine, don't smoke, get Vitamin D, start walking or other weight bearing exercise, get your calcium from high absorption sources.
Here's some links I looked up on Google for evidence, by doing a search on "milk" and "osteoporosis". I bet you could find similar evidence by searching on "protein" and "osteoporosis".
www.strongbones.org
www.pcrm.org/health/Preventive_Medicine/strong_bones.html
www.milksucks.com/osteo.html
http://www.greaterthings.com/Editorial/Milk_Osteoporosis.htm
www.cyberparent.com/nutrition/osteoporosiscalciumprotein.htm
.newcenturynutrition.com/public_html/webzine/archives/whatif.shtml
milk.elehost.com/html/osteoporosis.html
milk.elehost.com/html/why_does_calcuim_leave_the_bon.html
This is a start, I encourage you to explore this topic, it's very interesting and relevant to us all! :)
--------------------------------
Teeth Grinding
[http://flfl.essortment.com/grindingteeth_ryvp.htm]
People with bruxism [Teeth Grinding] have noticed that the more stress they have the worse it gets. It is important to take B vitamins to keep your stress levels down. But most often it is a vitamin deficiency that is causing bruxism. Taking calcium and pantothenic acid can prevent bruxism. Calcium is used in the muscles to stop involuntary movements. Pantothenic acid maintains muscle coordination. This is not medically proven, however.
Fluctuations in blood sugar levels may be involved.
Stress, tension, and anxiety are often the cause of tooth-grinding.
Suppressed anger or frustration.
Aggressive, hyperactive, or competitive personality type.
Hypoglycemia, related to low adrenal function, is often the cause of bruxism. Follow a hypoglycemic diet.
RISK FACTORS MAY INCREASE WITH:
Increased stress, tension and anxiety. / Hyperactive personality type. / Stimulants such as tobacco and caffeine may cause your body to produce more adrenaline, which may worsen bruxism.
-----------------------
FLUORIDE & FLUOROSIS
Symptoms of fluorosis include:
- tooth discoloration
- white or brown chalky spots
- brown enamel
- pitting of teeth
- excessive wear on the enamel
- structural damage to the enamel
- brittle teeth in which the enamel breaks easily
|
Hypoplasia is an erosion of the enamel. Also known as "mottled" teeth, this is often indicative of fluorosis: enamel surfaces of the teeth are subject to attrition and show marked wear. Brown stain is frequently a disfiguring feature.
- Colquhoun J. Community Health Studies 11:85-90 1987. [ From: http://emporium.turnpike.net/P/PDHA/fluoride/blunder.htm ]
----------------------
From www.merck.com w/ Long URL]
Defects in tooth enamel may be caused by abnormal calcium metabolism associated with rickets, which results in enamel hypoplasia. A rough, irregular band forms in the enamel when abnormal calcification occurs. Any prolonged fever illness during odontogenesis (the formation of "dentin" and "cementum," natural strengthening processes) can produce a permanent narrow zone of chalky, pitted enamel, visible after the tooth erupts. Thus, the age at which the disease occurred and its duration can be estimated from the location and height of the band. Amelogenesis imperfecta (teeth are covered with thin, malformed enamel) causes severe enamel hypoplasia. Chronic vomiting (as in bulimia) decalcifies the dental crowns, primarily the tongue-level surfaces of the lower anterior teeth.
Treatment of all these conditions consists of extensive restorative dentistry, particularly artificial crowns ["Uh-uh, No Sale" -rj], after the cause is removed or corrected. Swimmers who spend much time in overchlorinated pools lose considerable amounts of enamel. If the pool water is buffered, brown calculus deposits form; they can be removed by dental cleanings.
----------------------
[From: http://libaware.economads.com/daretothink.php ]
Hundreds of millions of people have developed Dental Fluorosis or Crippling Skeletal Fluorosis. . . not necessarily from fluoridated water, but from fluoride -- regardless of the source.
The U.S. Public Health Service says fluoride makes dental enamel more porous, and makes bone more brittle.
-----------------
[ From: bcd.tamhsc.edu/cedental/div5sec5.HTM ]
Heavy use of fluoridated toothpaste up to age 8 may be a risk factor for dental fluorosis.
COMMENTARY
For the past half century, questions have been raised about fluorosis and fluoride ingestion. We have seen the effects from geographic areas with heavy natural fluoride in the water, and many reports suggest that the prevalence of mild fluorosis is increasing in both fluoridated and non-fluoridated areas. New understandings of appropriate levels of fluoride help us monitor total intake on behalf of the patients in the communities we serve.
----------------------------
[http://www.fluoride.org.uk/news/fluoride_victims/colgate_payout.htm ]
The £1,000 paid in Kevin Isaacs's case relates to the expected cost of coating his teeth after the mottled enamel has been removed.
A LEADING toothpaste manufacturer has paid £1,000 to a child whose teeth appear to have been damaged by fluoride. In what is believed to be the first such case, Colgate-Palmolive made a "goodwill" payment after an independent specialist diagnosed the boy as suffering from a condition linked with fluoride. At the same time The Telegraph has also learned of research, kept hidden in America for 50 years, suggesting that fluoride can damage the central nervous system and teeth.
-----------------------
REMINERALIZATION
& DEMINERALIZATION
A cavity (hole) occurs when the calcium in the tooth enamel has been removed by repeated acid attacks. The enamel can no longer repair itself through the natural remineralization process.
------------
WHAT IS DEMINERALIZATION?
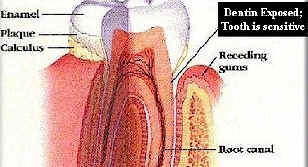
Demineralization is the process of removing minerals, in the form of mineral ions, from dental enamel. "Demineralization" is another term for "dissolving the enamel." Dental enamel is a crystalline latticework composed of various minerals, the principal component of which is a complex calcium phosphate mineral called hydroxyapatite ("hi-drox-e-appetite"). A substantial number of mineral ions can be removed from hydroxyapatite latticework without destroying its structural integrity; however, such demineralized enamel transmits hot, cold, pressure and pain much more readily than normal enamel. For example, if you feel something like a toothache, but the dentist says you don't have a cavity, chances are good you are feeling the results of a severely demineralized spot on your tooth that hasn't yet formed a cavity. Your dentist may also tell you that your enamel is soft at that spot, and that s/he can actually penetrate your enamel with a probe.
WHAT IS REMINERALIZATION?
Remineralization is the process of restoring minerals - again, in the form of mineral ions - to the hydroxyapatite's latticework structure. Remineralization is like replacing the missing rungs in a rickety ladder to make it strong and stable again - except that remineralization is three-dimensional, and the lost "rungs" (i.e. different mineral ions) must be replaced with "rungs" having the exact same shape, size and the same electrical charge as those lost from the lattice. Both remineralization and demineralization occur on the surface of the tooth. If you examine the cross-section diagram of a tooth, you will see there is no connection between the bloodstream and the enamel. Therefore, taking mineral supplements has virtually no impact on remineralizing the teeth. (It's also worth noting that this is true in reverse too: An event that draws on minerals in the blood, such as pregnancy or healing a broken bone cannot extract minerals from the teeth, as is widely believed.).
WHAT CAUSES DEMINERALIZATION?
Strong, stable acids, mostly: To a certain extent, these are found in acid foods, such as tomatoes or oranges; but they're also formed by oral bacteria that feed on starches and sugars in your mouth, especially refined sugars, secreting acids as by-products.
WHAT CAUSES REMINERALIZATION?
This natural mechanism is enhanced be eating unprocessed foods, rich in minerals, including trace minerals, such as natural and organic foods.
WHAT IS THIS NATURAL REMINERALIZATION MECHANISM?
Our bodies utilize carbon dioxide from our breath and water from our saliva to create a mild, unstable acid, carbonic acid.
FIRST, sufficient minerals must be present in the saliva. Since foods are the principal source of minerals for the teeth, an adequate diet, or insufficient time chewing foods (which transfers minerals to the saliva) may result in mineral-poor saliva. SECOND, a molecule of carbonic acid must be produced. Only a miniscule fraction of the carbon dioxide from the breath is converted to carbonic acid. THIRD, the carbonic acid molecule must be produced in proximity to a mineral molecule, which it then dissolves into its ionic components. As you can see, natural remineralization is a pretty "iffy" occurrence. In contrast, demineralization is enormously accelerated by the refined sugars and processed foods in most of our diets.
-------------------
Veneers
Once you have veneers, you cannot reverse the treatment, because a part of your enamel has been removed. And until the veneers are attached to your teeth, they may be sore and look strange.
If a veneer chips or peels off, or if a cavity forms under a veneer, the veneer must be redone. The other option is to put a crown on the tooth.
Veneers are stronger than bonding. They are also less likely to change colour or stain. Porcelain veneers are stronger than acrylic veneers.
Veneers can chip or peel off if you do not take care of them. Don't bite your fingernails or chew on hard objects.
On your first visit, your dentist may give you freezing (called a local anesthetic). He/she then removes part of the enamel from your teeth to make room for the veneers. Your dentist makes a mold (or an impression) of your teeth. The impression is sent to a dental lab, where your veneers are custom-made.On the next visit, your dentist puts a mild chemical on your teeth to make them a little rough. This helps the veneers stick to your teeth better.The veneers are then attached to your teeth one by one, using composite resin cement.
-----------------------------------------
Crowns, etc
[www.dentalcomfortzone.com/archive/BrokenDenturesCrowns.html.]
You can temporarily remedy this problem by using temporary dental cement found at the drug store, and carefully re-cementing the crown. This may not be necessary if you can get to the dentist within a day or two. Never wait more than a few days to get a crown re-cemented. Teeth move and shift very quickly without the crown in place. Sometimes it is not possible to reuse the crown if the teeth have shifted significantly, requiring the dentist to have to make a new crown.
------
Dentemp® O.S.: This FDA Approved Over-the-Counter Dental Cement / CVS $3.99
------------------------
Tooth Enamel Erosion
 When enamel is eroded, the tooth is unprotected and decay occurs. A filling is man's attempt to replace lost enamel. Once enamel is gone, it doesn't get restored - it's gone forever; cavities will form, causing brownish discoloration, softer tooth surface, and eventually cracking. So, what do you do when your enamel has been stripped away but you want to keep your teeth?
When enamel is eroded, the tooth is unprotected and decay occurs. A filling is man's attempt to replace lost enamel. Once enamel is gone, it doesn't get restored - it's gone forever; cavities will form, causing brownish discoloration, softer tooth surface, and eventually cracking. So, what do you do when your enamel has been stripped away but you want to keep your teeth?
They say: After the enamel is gone, other than pulling what's left of the teeth, there isn't much dentists can do. Enamel Treatments: Cements, Polymers... (on this page)
[ www.dentalgentlecare.com/sensitivity.htm ]
Causes of sensitive teeth: ...Long term use of mouthwashes such as Listerine or Oraldene damage dentine and cause dentin sensitivity and reverse the beneficial effects of toothpaste ...Dehydration due to diuretics such as alcohol beverages, caffeine-containing drinks like coffee and Mountain Dew...
What to you once you already have sensitive teeth:
Use a toothpaste for sensitivity. They work in a cumulative fashion to cover the open tubules. They contain strontium chloride and/ or potassium nitrate which act to remineralize the tooth surface by diffusing into the open pores (tubules) on the enamel. This process helps block transmission of sensation from the tooth surface to the tooth nerve. They need to be used 4-6 weeks before any changes can be noted. / Chemical desensitization (Gluma/ Hurriseal / Pain-Free) provided by your dentist is the most common method of treatment. /
Surface sealers or self etch primers (Seal & Protect/Clearfil SE Bond ) can be a costly.
Enamelon ~has a Liquid CalciumTM formula, which combines the active strength of sodium fluoride with soluble calcium and phosphate ions to strengthen weakened tooth enamel.
[Note: The product intimates that enamel can be rebuilt, which is impossible. Once enamel is gone, it's gone for life.]
[www.floss.com/q4.htm.]
..Enamelon, Inc.was founded in 1992, and developed a toothpaste that helps remineralize tooth enamel and, thus, hardening the tooth. This aids in decreasing cavities. It works by using soluble calcium, phosphate and fluoride. According to their research, this toothpaste stops cavities before they can form. It also reverses early stages of tooth decay. Studies have been performed at SUNY, Stony Brook to evaluate if it also decreases dentinal tooth sensitivity. What was concluded was that enamelon did in fact decrease tooth sensitivity.
--------------
Enamel Treatments, Dental Restoration
COMPSITE BONDING
http://www.fluoridealert.org/dental-fluorosis.htm
Treatment options for fluorosis vary and will depend in part on the severity and what you can afford (some of the treatments are very expensive). Some of the more common treatments include:
"Composite bonding": Composite bonding first involves lightly roughening the area of the damaged enamel. After etching the enamel, a composite resin (with a color matching your teeth) is "glued" on to the exterior of the tooth. Less expensive than veneers and crowns.
• Cost: Composite tooth bonding averages $200 to $500 per tooth.
• Results: Very large bonding restorations can break and stain if the individual is not careful with them, but in most cases, tooth bonding will last from 3 to 7 years.
http://www.massasoitdental.com/gallery/default.asp Massasoit Dental, 288 Belmont Street,
Brockton, MA 02301.
508.583.0103
Google - "Composite Bonding" messages
www.owlnet.rice.edu/~chem152/lab152/polymers/therms.pdf.
Polymers are used to seal porous teeth and reconstruct missing enamel.
Treatments range from preventive care using sealants and bonding for esthetics to extensive removable and fixed prosthetic reconstruction. (Permanent dentition) ages 11 and older.
---------------
Types of Restorative Materials
[ From: bcd.tamhsc.edu/cedental/div5sec5.HTM ]
glass-ionomer restorative materials, such as glass-ionomer-silver-cermet cement, shows that this newer material has improved physical characteristics such as improved wear resistance and fracture toughness. They hypothesize that the hardened material may have better resilience than earlier glass-ionomers, thus conferring the improved fracture resistance.
The authors use light-hardening glass-ionomer-resin cement to restore Class I, Class III, Class V, and certain conservative Class II lesions. They do not recommend this material for Class II lesions in permanent teeth because of the untested challenge of increased biting forces. In addition to their perception of better physical properties, the authors endorse this material because of its quick initial hardening for easier handling. The authors acknowledge that more long-term assessment is needed and they recommend that primary teeth can best serve as this "proving ground."
-------------------
Different Enamel Applications & Compunds
Categories were divided into the following enamel treatment groups (10 teeth each):
Group 1 (control) - etched with 37% phosphoric acid;
Group 2 - air abraded with 45 mm particles of sodium bicarbonate;
Group 3 - air abraded with 50 mm aluminum oxide particles;
Group 4 - etched with 2.5% nitric acid;
Group 5 - air abraded with sodium bicarbonate particles and etched with 37% phosphoric acid; and
Group 6 - air abraded with 50 mm aluminum oxide particles and etched with 37% phosphoric acid. Following the enamel treatment, a sealant was bonded to the surfaces.
----------
Materials - Enamel Treatments
a disto-occlusolingual Class II restoration using light-hardening glass-ionomer-resin cement (Fuji II LC, GC America).
From: http://www.cnn.com/HEALTH/library/DA/00013.html
DIABETES & TEETH
( Google Search: "diabetes can" "tooth decay" 031605)
Tooth and gum damage: Diabetes can take steady toll
Day in and day out, high blood sugar caused by diabetes can contribute to accumulating damage to your gums and teeth, which may cause tooth loss. Here's how it happens:
Plaque: How diabetes feeds this cavity-causing menace
An invisible film of bacteria, saliva and food particles (dental plaque) normally covers teeth. The bacteria feed on the sugars and starches in the foods and beverages you consume and produce acids that damage the hard enamel coating of your teeth.
High blood sugar levels in diabetes give the bacteria a greater supply of food, allowing them to produce even more acid. The damage from this acid increases the possibility of tooth decay (cavities).
Gum disease: From irritation to tooth loss
Plaque can cause other problems, too. If you don't remove it from your teeth with regular brushing and flossing, it hardens under your gumline into a substance called tartar.
Tartar irritates the gums, causing a condition called gingivitis. This makes the gums tender, swollen and red, and they may bleed when you brush your teeth. Fortunately, your dentist can prevent or treat gingivitis by removing tartar during a professional dental cleaning.
However, untreated gingivitis can lead to a more serious condition in which bacteria infect your gums and the bones around your teeth (periodontitis). This can cause your gums to pull away from your teeth and your teeth to loosen and even fall out.
Gingivitis and periodontitis are the most common oral complications of diabetes. If you have type 2 diabetes, you're three times more likely to develop gum disease than is someone who doesn't have diabetes. Diabetes lowers your body's resistance to infections and slows your ability to heal.
* * * * *
Q. How does diabetes affect oral health?
A. Diabetics are at greater risk for multiple oral health problems. Diabetes reduces the body's resistance to infection, and gum tissues are often affected. In fact, periodontal disease appears to be more frequent and more severe among those with diabetes. Diabetic patients often complain about a dry mouth that will increase the possibility of tooth decay and gum disease. They also are susceptible to oral fungal infections.
Gum disease and diabetes
Gum disease is an infection that can start when bacteria that is normally present in the mouth begins to form a sticky plaque on the tooth's surface. If this isn't removed effectively on a regular basis, it can trigger gingivitis (gum inflammation). Symptoms are red, swollen and bleeding gums, which are often painful. If left untreated, gingivitis can then develop into gum disease, which can be closely linked with tooth decay.
High blood glucose levels will encourage an infection to spread anywhere that it occurs in the body, including in the mouth or gums. This is why it's important to keep your blood glucose levels well controlled.
* * * * *
www.nyp.org/health/cd_rom_content/adult/diabetes/oral.htm
Diabetes can also cause other oral problems, including:
THRUSH:
Thrush, a fungal infection of the mouth, occurs more often in persons with diabetes because of high sugar levels in the saliva, as fungus thrives on glucose.
DRY MOUTH:
Often a symptom of undetected diabetes, dry mouth means the mouth does not have enough saliva to keep itself wet. Saliva is necessary to help digest food, and prevent infection and tooth decay by controlling bacteria and fungi. Dry mouth can make tasting, chewing, and swallowing food difficult, and can impede speech. In addition, dry mouth can cause mouth infections and tooth decay.
Periodontal Disease
& Trench Mouth
GUM HEALING
Google: "periodontal decay"
From: http://www.ismilepeabody.com/services/periodontics.asp
Gum problems include:
• Gingivitis is an inflammation of the gingiva.
• Periodontitis is a more serious form of gingivitis.
• Plaque is a thin film of food particles and saliva. It feeds bacteria, causing tooth decay.
• Tartar is hardened plaque.
• pockets (when the collar of gum becomes infected and detaches from the tooth, the space it leaves is called a pocket);
• bleeding (gums should not bleed regularly and is an early sign that pockets and bone loss will occur);
• bone loss (if left untreated bone loss due to periodontal decay can lead to teeth removal);
• abscess (the expansion of a gum pocket due to trapped bacteria.)
Trench Mouth
• Trench mouth is a painful form of gingivitis (gum inflammation). It a bacterial infection of the gums. It occurs when there is an excess of normal mouth bacteria, causing infection.
Trench Mouth Symptoms include: Painful gums; gum bleeding from any pressure or irritation; Gums appear reddened and swollen; Crater-like ulcers between the teeth; Foul taste in the mouth; Bad breath. Symptoms often begin suddenly.
Trench Mouth Treatment: (goals of treatment are cure of the infection and relief of symptoms.)
• have teeth professionally cleaned, with thorough plaque removal. Dental cleanings may be recommended on a regular basis until the disorder is cleared.
• IRRIGATION. Good oral hygiene is vital to the treatment of trench mouth. Irrigate the affected area with a Water Pic.
• Brushing & flossing twice a day or more.
• Antibiotics "if there's a fever". [Indicating DESTRUCTION OF BACTERIA is key to healing. Consider: Listerene, UT, Water Pick... -rj]
• Salt Water Rinses "to soothe pain..."
• Massage gums - 15 minutes per day; use eucalyptus, witch hazel, or vitamin E; rub finger a in circular motion along the gum line.
- • Hydrogen peroxide to rinse or irrigate the gums, to remove decayed gum tissue. Mouthwashing with hydrogen peroxide may be needed to ensure that the gums heal completely.
- [Using hydrogen peroxide as mouthwash has been shown to help clear up periodontal disease that may already have taken hold.]
• Merck Manual recommends diluting 3% hydrogen peroxide with 50% water, as part of a treatment for trench mouth. Overuse may damage cells and soften tooth surfaces.
• 2 minutes two to three times a day. [Ordinary use; Trench Mouth situations still pending. Remember the "irrigation" - Water Pick & Peroxide; - rj]
• Hydrogen Peroxide page - www.stretcher.com/stories/03/03jan06j.cfm
• Toothbrushes should be changed monthly, since bacteria accumulates on them.
• Irritants must be avoided, including smoking and hot or spicy foods
• More serious forms may require Dental surgery to remove plaque, tartar, and infected gum tissue.
• Vitamin C is important in maintaining healthy gums.
•Calcium and magnesium are recommended to minimize the loss of bone in gum disease.
The infection usually responds to treatment. It can be quite painful until it is treated. If left untreated, the infection can spread to the cheeks, lips, or jawbone and destroy these tissues.
The main cause of periodontal disease is bacterial plaque which produces toxins that irritate the gums, causing swelling and bleeding. It constantly forms on the teeth and if it is not removed by daily brushing and flossing will harden into calculus (tartar).
Additional causes of gum disease are smoking, stress, diabetes, poor nutrition, medications, and grinding one's teeth.
---
Q: I have increasing pain below the gum line. The pain is dull but intense and is lessened but not relieved by anti-inflammatories and OraGel.
A: It is possible that some piece of food got caught under the gum and now normal bacteria in the mouth is beginning to percolate. The pain is not caused by a shift of the teeth but from increased pressure from inflammation.
• GUM MASSAGE
• Periodontists recommend daily gum massage as a primary treatment for gingivitis and periodontitis. Gum massage enhances blood flow, which leads to improved gum health. Gum massaging firms up gum tissue to help prevent, control and actually reverse periodontal disease.
---
Try a warm saltwater rinse. "Take a few swigs of warm salt water and swish it between your teeth and gums," advises director of periodontics at Temple University, Philadelphia. "It has a general soothing effect. If you have an abscess, the salts will help draw it out and drain it." He recommends one teaspoon of salt in a glass of lukewarm water. (Salt water is also your first line of defense for any gum burn, cut, abrasion or wound.)
---
www.1sthealthsource.com/articles/teeth/teeth.html
Nightly gum packs made from herbs rolled in gauze tucked into the corners of his mouth.
• Turmeric, aloe, willow bark, vitamin E, and powdered alum did the trick. He noted a "significant turnaround," and by the four- month mark was out of crisis.
• "Turmeric fights gum inflammation by halting the action of a gene that creates irritant chemicals. " - www.nutritionalwellness.com/columnists/heller/
• You can buy powdered turmeric in supermarkets. If you get it in the spice section of the market, it will cost you some bucks. In Indian markets, you get more for your money.
• Brush teeth with a mixture of powdered alum and salt.
• Periodontal disease (PD) is a long-term, low-grade bacterial infection of the gums, bone, and ligaments that support the teeth.
Reversing Gum Disease Naturally - book - Amazon - ISBN: 0471222305
http://www.mothernature.com/Library/bookshelf/Books/48/95.cfm
Grip an area of your gums between your thumb and index finger (index on the outside) and rub the top and bottom gums. A few minutes' massage every day, all around the top and bottom gums, should help stop gingivitis.
Daily gum massage improves blood circulation. That can help make gums more resistant to gingivitis and other gum disease.
TO: HOME PAGE - Main Index
 When enamel is eroded, the tooth is unprotected and decay occurs. A filling is man's attempt to replace lost enamel. Once enamel is gone, it doesn't get restored - it's gone forever; cavities will form, causing brownish discoloration, softer tooth surface, and eventually cracking. So, what do you do when your enamel has been stripped away but you want to keep your teeth?
When enamel is eroded, the tooth is unprotected and decay occurs. A filling is man's attempt to replace lost enamel. Once enamel is gone, it doesn't get restored - it's gone forever; cavities will form, causing brownish discoloration, softer tooth surface, and eventually cracking. So, what do you do when your enamel has been stripped away but you want to keep your teeth?